
When Craig Settee explains the importance of kidney screening to members of Indigenous communities in B.C., it comes from several points of view. He is the coordinator of the Indigenous Peoples’ Engagement and Research Council (IPERC) at Can-SOLVE CKD, a pan-Canadian patient-oriented kidney research network. He is also a living kidney donor to his brother, and he is Anishinaabe (Ojibwe) on his mother’s side and Nehinaw (Cree) on his father’s side.
“I’m doing this work because it has affected my family firsthand. Bringing this to share with others is important so other families and community members who may have kidney disease can identify it earlier,” says Settee. “We know kidney disease affects Indigenous people at a higher rate than other people in the country. We need to take steps to close the gaps.”
Burden of kidney disease much higher in Indigenous communities
The statistics are alarming: while one in 10 Canadians have chronic kidney disease (CKD), the rate for Indigenous adults is one in three. This is due in part to high rates of diabetes. That’s where Kidney Check comes in. A partnership between Can-SOLVE CKD and the First Nations Health Authority launched in 2019. It’s a screening, triage, and treatment research program with Indigenous communities in rural and remote parts of Canada.

CHÉOS Scientist Dr. Adeera Levin is co-principal investigator at Can-SOLVE CKD. She says, “The aim is to prevent CKD and diagnose it early. We want to identify those at highest risk so they can receive treatment before it becomes kidney failure.”
Kidney Check program is entirely community-led
The process of setting up Kidney Check in each community usually starts with a community engagement session, often sharing a meal, a blessing and welcome from an Elder or Knowledge Keeper, and a presentation, followed by questions from members. It’s a non-clinical environment that is tailored to each community. Then the health care providers do the actual screening. This involves a blood pressure check, finger poke for diabetes screening, and a urine sample. At the third and final visit, the community evaluates the program and provides feedback.
“This is community-based, nation-led. We honour self-determination of the community,” explains Catherine Turner, Kidney Check senior research coordinator. “It really is quite in contrast to how health care has been carried out with Indigenous people, especially when you think of all the trauma and racism that has been a part of the experience.”
Settee elaborates further, “Indigenous people are the main speakers, presenters, and health care providers for Kidney Check. We need to amplify our voices and experiences, and openly share any hesitancy and discomfort that comes from that so we can encourage others to be involved.”
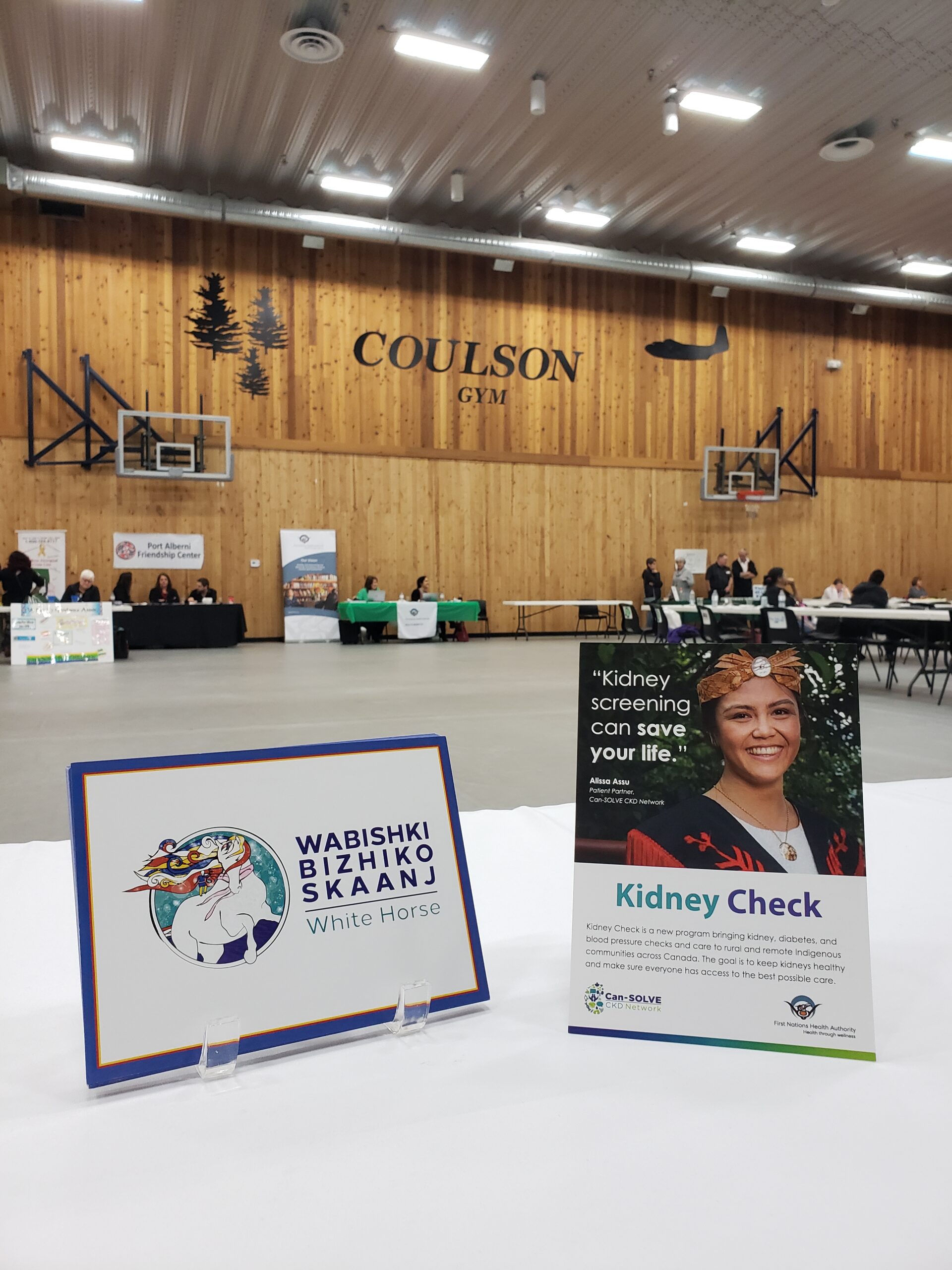
Seeing themselves reflected in the health care experience is vital to forging trusting relationships between Indigenous people and providers, explains Turner, who is Métis. She points to the Kidney Check poster as an example. It features Alissa Assu, a kidney transplant recipient from Campbell River, wearing her regalia.
“Indigenous people are going to be curious about it. They see themselves, or someone similar to them, and it sparks a conversation about it,” says Turner.
Health research shifting to include Indigenous perspective
Settee’s patient family experience started when he was young. His brother Kevin was 10 when he was first diagnosed with kidney disease. This led to a kidney transplant nearly a decade later. At some point, Settee remembers his brother getting asked to take part in a medication study. It was a family friend who was the nurse doing recruitment. That helped the family feel comfortable with the process of participating or not. He knows that hasn’t been the norm for many other Indigenous people, but he is hopeful things are changing as researchers engage with Indigenous patient partners, take cultural safety training, and learn from Indigenous experiences.
“If that research will eventually affect Indigenous people, it is so important for researchers to have some knowledge on Indigenous ways of knowing, and how to properly collect and care for data from Indigenous patients and communities,” Settee remarks.

Going virtual during the pandemic
Kidney Check had just gotten underway in a few provinces, including B.C., when COVID-19 hit. In-person visits were halted, but the team added a virtual screening option for communities that wanted to try an online program until community visits could resume.
Turner is hopeful they will be able to get back into communities at the end of September, starting with the Nuu-Chah-Nulth nation on Vancouver Island. They have set a goal of screening about 300 Nuu-Chah-Nulth members by the end of this year.
Despite the slow start, the impact has already been noticeable. Turner shared the story of one young teenager who had no symptoms at all, seemingly in good health. Once she was assessed, she actually presented as medium-to-high risk. Now that girl is connected to a nephrologist.
“Kidney Check takes the fear away from being screened. People have a far better understanding of what CKD is, they appreciate learning more about their kidneys, and having an opportunity to speak to the doctor in a non-clinical environment,” comments Turner. “They tell us to keep coming back!”



