With over 165,000 health and wellness apps available, technology’s permeation into health care has earned the name “e-health”, and offers to help patients track and manage their conditions with some digital help, ranging from pop-up notifications about exercise goals to an AI therapist.
At CHÉOS, Scientists Drs. Linda Li and Michael Krausz are developing and researching e-health in two very different fields — arthritis care and mental health, respectively.
Though their disciplines seem worlds apart, their e-health research brings up common notions about how technology will impact patients and health care delivery: It could increase access for remote and underserved populations, build overall capacity and deliver more timely care, and empower patients to better manage their conditions.
We talked to Drs. Li and Krausz about the role of consumer technology in their fields and their research interests in the realm of e-health.
Step Up Notifications: Digital Tools in Arthritis Care
Dr. Li, Senior Scientist at Arthritis Research Canada, first engaged with e-health when she began doing research on how patients make decisions regarding different treatment options.
“We started looking at options to help people make better treatment decisions and recognize that they need to go to a doctor in a timely manner,” said Dr. Li. “So, we started to develop patient decision aids.”
In a collaboration with students from the Centre for Digital Media in Vancouver, Dr. Li’s team developed an interactive patient decision aid to present the latest evidence about a common arthritis medication.
“We tested it and found that it actually helped people to make better decisions and feel less conflicted,” said Dr. Li, pointing to results from a proof-of-concept study of ANSWER-2, which CHÉOS’ Dr. Nick Bansback co-authored.
Prior research Dr. Li has been involved in showed that when patients used the internet to learn more about their conditions, their interactions with health care providers changed—patients were more likely to engage in a discussion with their doctor, rather than have the treatment plan dictated to them. She believes wearable devices and health apps could further empower patients.
“Knowing your own body gives you a lot of power when you go to see your doctor, in terms of knowing exactly what to convey about what you feel is out of the ordinary, and to engage in a discussion,” said Dr. Li. “Some of the patients we’ve interviewed talk about a more level playing field.”
Investigating the use of digital media to help patients make decisions spring-boarded Dr. Li into projects that examine how to incorporate technology and digital media into knowledge translation and arthritis care, such as how to leverage the use of wearable devices, like a Fitbit, in physical therapy and exercise promotion.
For example, Dr. Li served as the medical consultant and scientific lead for the development of Walk10Blocks, an iOS app that encourages sedentary people to walk at least 10 blocks a day.

On the surface, the app is an incentive to move, with motivational pop-up notifications and badges that can be unlocked with various levels of activity. However, research questions built into the app are collecting data on how users interact with the app—how often they open it, whether they complete the surveys, and more—that can be useful for improving the app and building more digital tools to prompt people to alter their behavior and assume healthier habits.
Moreover, at the BC Support Unit, an organization for patient-centred research, Dr. Li leads a group responsible for advancing the science in knowledge translation and implementation. Her team collaborates with the Unit’s Data Sciences and Health Informatics Cluster to develop an infrastructure for large databases, which can combine patient-reported data (such as Fitbit data) with administrative health care data. Such a data set could further knowledge of disease progression and management, as well as identify gaps in care and opportunities for intervention.
“When you incorporate patients’ experiences, which are collected on a day-to-day basis or over a long period of time, in a big database, you may actually see trends that nobody has thought of,” said Dr. Li. “That’s where I see e-health research going, not only improving care for patients—faster and more accurate screening, diagnosis, better management, better access to care—but also asking better research questions in a way that is truly meaningful.”
Dr. Li is currently testing a fitness tracking web app FitViz in clinical trials and recruiting patients for studies involving wearable devices.
Head in the Cloud: Online Mental Health Care
-
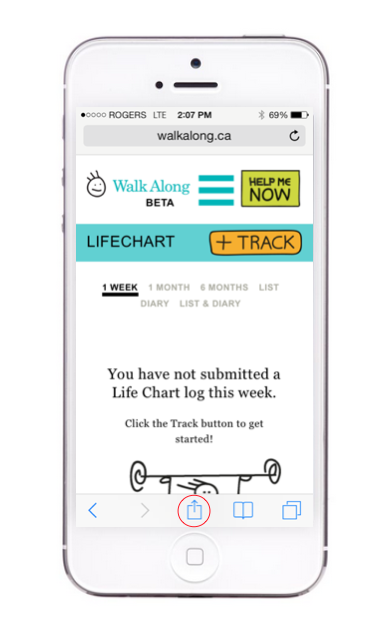
Screenshot via WalkAlong.ca
Dr. Krausz saw the potential of technology in health early on; he has been organising conferences on the use of computers in medicine for about 30 years. He made international headlines in the aftermath of the 2017 European Congress on Psychiatry for advocating for the urgent expansion of e-mental health services to address the shortcomings of traditional care.
“We have a huge gap in capacity and the current system is unable to provide care for the majority of patients,” said Dr. Krausz. He pointed to a recent World Health Organization survey of 21 countries which showed that only 16.5 per cent of individuals with major depressive disorder received “minimally adequate treatment” within a year.
Problems with access to mental health care are present in Canada too.
One recent Canadian study on mental health care needs found that gaps in care remain: Two-thirds of people with substance use disorders were not receiving care, and individuals with structural vulnerabilities—people born outside Canada, ethno-cultural minorities, those with lower education and income, and the elderly — were less likely to access services.
Timely care is an issue too. In B.C. in particular, patients referred to a psychiatrist wait 50 per cent longer than the recommended standard wait time, according to research by the Fraser Institute.
“That leads to the key question: Where is the future of mental health care, and for other areas of medicine like primary care?” Dr. Krausz said of the treatment gaps. “The only option I see, based on the current development in communications, is to use web-based tools to build capacity—through online resources and assessments; to run services through virtual clinics.”
With this vision for the future, Dr. Krausz, along with CHÉOS Scientists Drs. Iris Torchalla and Greg Werker, surveyed youth who had experienced suicidal ideation and either depression or anxiety and asked them about what they wanted out of e-health resources. Their results showed that youth wanted online tools that would enable them to access peer support, professional help over chat, coping tools, and avenues for sharing experiences, while also preserving their privacy.
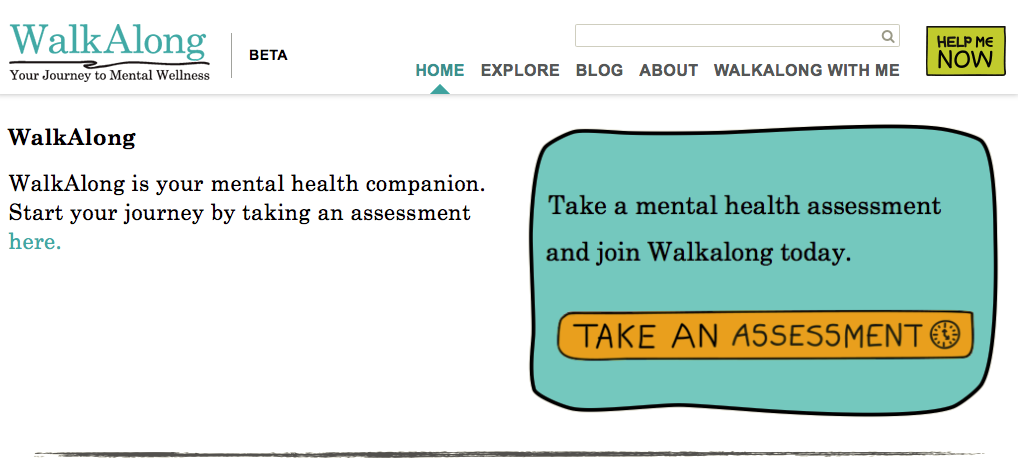
Dr. Krausz subsequently led the development of WalkAlong.ca, a youth-centred online platform where users can find educational and coping resources, assess their mental health, track their moods, and share experiences.
-
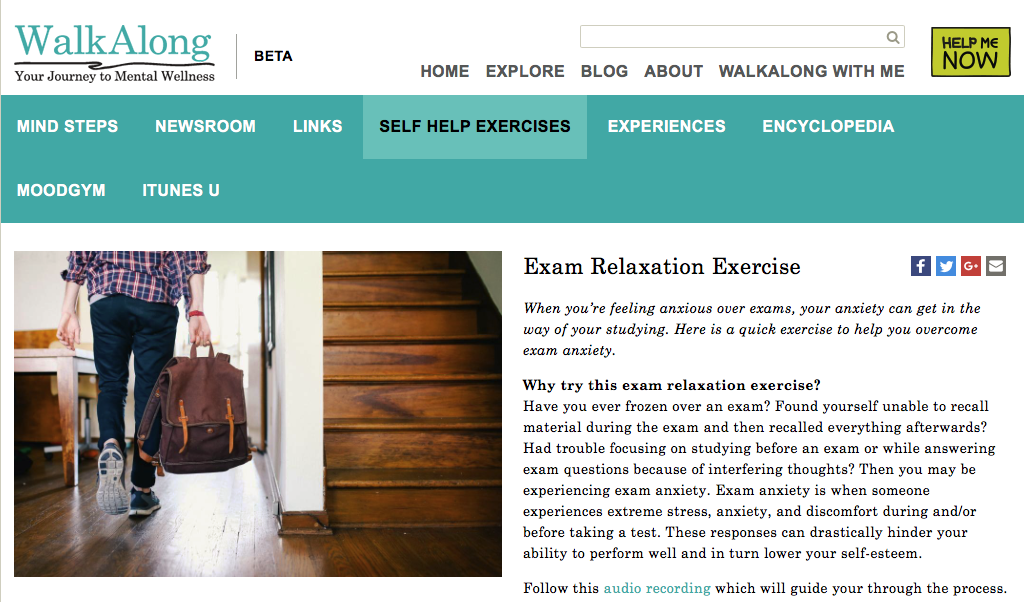
Screenshot via WalkAlong.ca
“The idea is to develop different functions that allow users to better deal with their problems,” said Dr. Krausz. “We are very much trying to work on empowering our patients—that’s a core principle.”
WalkAlong.ca currently focuses on mood disorders, but Dr. Krausz said he hopes to expand the platform to also provide resources for addiction, trauma, eating disorders, and more.
Dr. Krausz’ research interests lie in determining how e-health resources can help vulnerable populations, such as refugees, who do not have access to traditional care, and he plans to develop an online trauma platform geared toward them.
Additionally, observing students at UBC, where he is a Professor of addictions psychiatry, has prompted Dr. Krausz to also work on addressing youth and student mental health through an early intervention platform that can help youth before they reach a crisis point.
“The level of stress and stress-related psychopathology among students is unacceptable,” he said. “We have 10% of students having suicidal ideation—that shouldn’t be the new norm. We need to do something about it.”
-
Screenshot WalkAlong.ca
Dr. Krausz also organizes an annual conference on e-mental health hosted at UBC, where experts and people with experiences of mental health issues come together to discuss ways of growing and improving the online space for mental health support.
One aspect of the conference Dr. Krausz finds particularly valuable is the chance to learn from international experiences in adopting e-health.
“It’s exciting to learn from New Zealand, Australia, the Netherlands, and Germany, and see that it works and it works quickly,” said Dr. Krausz. “We need to encourage this paradigm shift in our country, not because it’s trendy, nice, and interesting, but because the majority of people in need—vulnerable people—don’t get the attention and care they need.”
The Questions Ahead
Not all questions surrounding e-health are purely research focused, however; experts and users alike have also brought up ethical concerns about regulation and privacy.
Both Health Canada and the U.S. Food and Drug Administration (FDA) only regulate apps that turn a phone into a medical device— for instance, if the app allows the phone to perform an electrocardiogram.
As a result, most health apps are not scrutinized for their efficacy.
While Dr. Krausz said he thinks patients should review mental health apps and thus have consumers be the judges of efficacy, Dr. Li noted that regulatory procedures could use an upgrade to catch up to technology’s impact on health care.
-
Illustration Courtesy MaRS
“The classification criteria were developed before we used apps, websites, and wearables for health care reasons, so I think some of the definitions will need to be updated to be more relevant to the kind of devices that we are using for the health care setting,” said Dr. Li. “Lots of work needs to be done and I think that’s where the ethical questions need to be dealt with in a thoughtful manner.”
Moreover, while personal devices could be indispensable epidemiological surveillance tools by virtue of collecting big data on various aspects of health, apps that monitor behavior could glean personal data that people may feel should be kept confidential and private.
Cases in which e-health devices have been used to make decisions about funding treatments or the cost of insurance are already setting a precedent for how such data can be used outside of research and improving care.
Like in other areas of science and technology, ethics and policy can have a hard time keeping up with the present scale of innovation in e-health.
“I think some of those [ethical] discussions need to happen more openly and rapidly because the technology is moving that way regardless of whether we like it or not,” said Dr. Li. “The better prepared we are, the more we can leverage the benefit and avoid the consequences when things blow up.”



