The Evidence Speaks Series is a recurring feature highlighting the latest in CHÉOS research. This series features summaries of select publications and is designed to keep media and the research community up-to-date with CHÉOS’ current research results in the health outcomes field. In recognition of Bell Let’s Talk Day, this month we are focusing on mental health research.
To ensure this research is quick and easy to share, we are now providing social cards that you are free to save and use as you see fit.
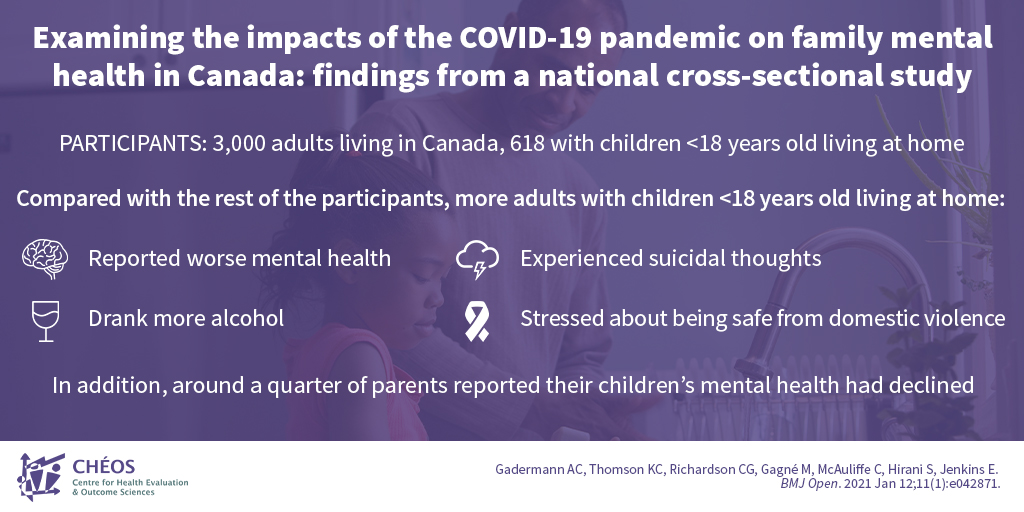
Canadian parents suffering worse mental health during pandemic than adults without kids
Gadermann AC, Thomson KC, Richardson CG, Gagné M, McAuliffe C, Hirani S, Jenkins E. Examining the impacts of the COVID-19 pandemic on family mental health in Canada: findings from a national cross-sectional study. BMJ Open. 2021 Jan 12;11(1):e042871.
CHÉOS Scientist Dr. Anne Gadermann and Program Head – Psychosocial Epidemiology Dr. Chris Richardson joined CHÉOS postdoctoral fellows Kimberly Thomson and Monique Gagné, plus a team from UBC School of Nursing, to investigate the impacts of COVID-19 on family mental health. Using survey data, the team discovered that almost half of parents with children aged under 18 reported worse mental health due to the pandemic. It was also reported that they drank more alcohol, felt more stressed about being safe from domestic violence, and experienced more thoughts about suicide and self-harm compared with the rest of the population. Furthermore, around one quarter of parents reported that their children’s mental health had worsened. These results could help inform policymakers and service providers about family needs during this trying time.
—
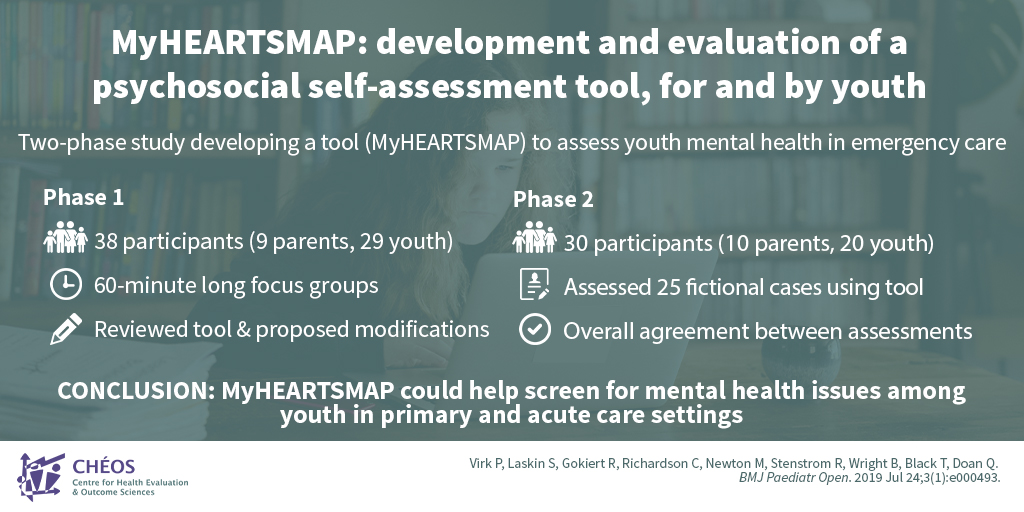
Youth helped develop online mental health screening tool
Virk P, Laskin S, Gokiert R, Richardson C, Newton M, Stenstrom R, Wright B, Black T, Doan Q. MyHEARTSMAP: development and evaluation of a psychosocial self-assessment tool, for and by youth. BMJ Paediatr Open. 2019 Jul 24;3(1):e000493.
In 2019, CHÉOS Program Head – Psychosocial Epidemiology Dr. Chris Richardson and Scientist Dr. Rob Stenstrom joined colleagues from UBC and the University of Alberta to develop MyHEARTSMAP — a self-administered online psychosocial assessment tool for youth — and evaluate its reliability. The team conducted hour-long focus groups where youth and parents reviewed the tool and advised on any modifications. Participants then underwent training and assessed 25 fictional cases to evaluate the tool. Here, there was agreement between assessments, supporting the tool’s reliability. Today, MyHEARTSMAP is being used to explore the impact COVID-19 on the psychosocial status of children and youth.
—
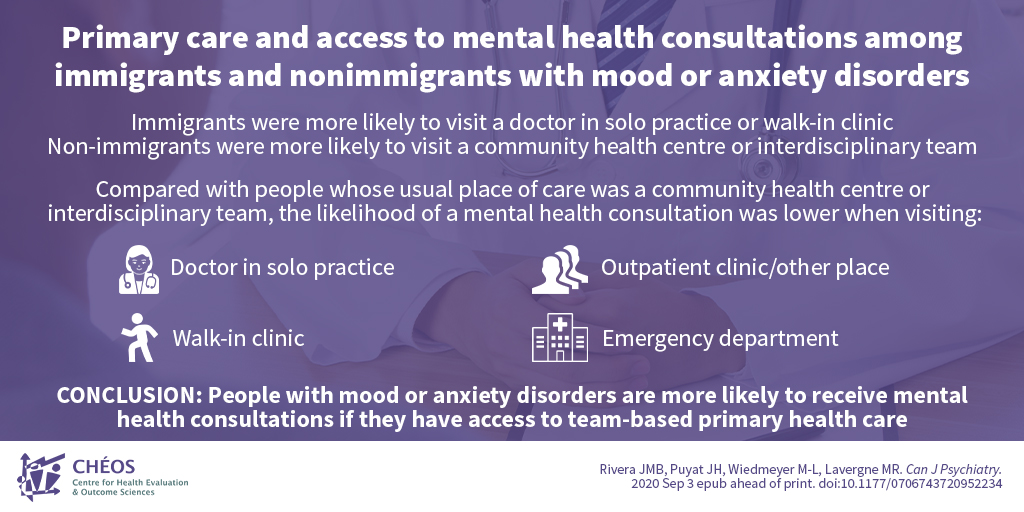
Immigrants in Canada are less likely to receive mental health consultations than non-immigrants
Rivera JMB, Puyat JH, Wiedmeyer M-L, Lavergne MR. Primary Care and Access to Mental Health Consultations among Immigrants and Nonimmigrants with Mood or Anxiety Disorders. Can J Psychiatry. 2020 Sep 3 epub ahead of print.
CHÉOS Scientist Dr. Joseph Puyat collaborated with researchers from UBC and Simon Fraser University to examine the relationship between usual primary care setting and access to mental health consultations among immigrants and non-immigrants with self-reported mood or anxiety disorders. Using data from the 2015 and 2016 Canadian Community Health Survey, the team analyzed data from 14,378 respondents with mood or anxiety disorders. Compared with non-immigrants, immigrants were more likely to obtain primary care from walk-in clinics or a doctor in a solo practice. The likelihood of receiving a mental health consultation in these settings was lower than in team-based primary care settings, which are more frequently attended by non-immigrants. These findings highlight that immigrants are less likely to receive a mental health consultation, and policies are required to increase access to team-based primary care and address the gap in mental health services access.